What is an Invisible Illness?
Table of Contents
What is an invisible illness
List of invisible illnesses
How common are invisible illnesses
Challenges of living with an invisible illness
How to support someone with an invisible illness
How to learn more about invisible illness
What is an invisible illness?
While there is no formal medical definition of an invisible illness, medical conditions are generally labeled an invisible illness when they are chronic, cause significant pain or fatigue, and are entirely or mostly invisible to the casual observer.
Most people with an invisible illness are women (meaning the sex they were assigned at birth), and there are tens of millions of Americans who live with at least one invisible illness. Virtually everyone is guaranteed to know at least one person with an invisible illness, whether they are aware of it or not.
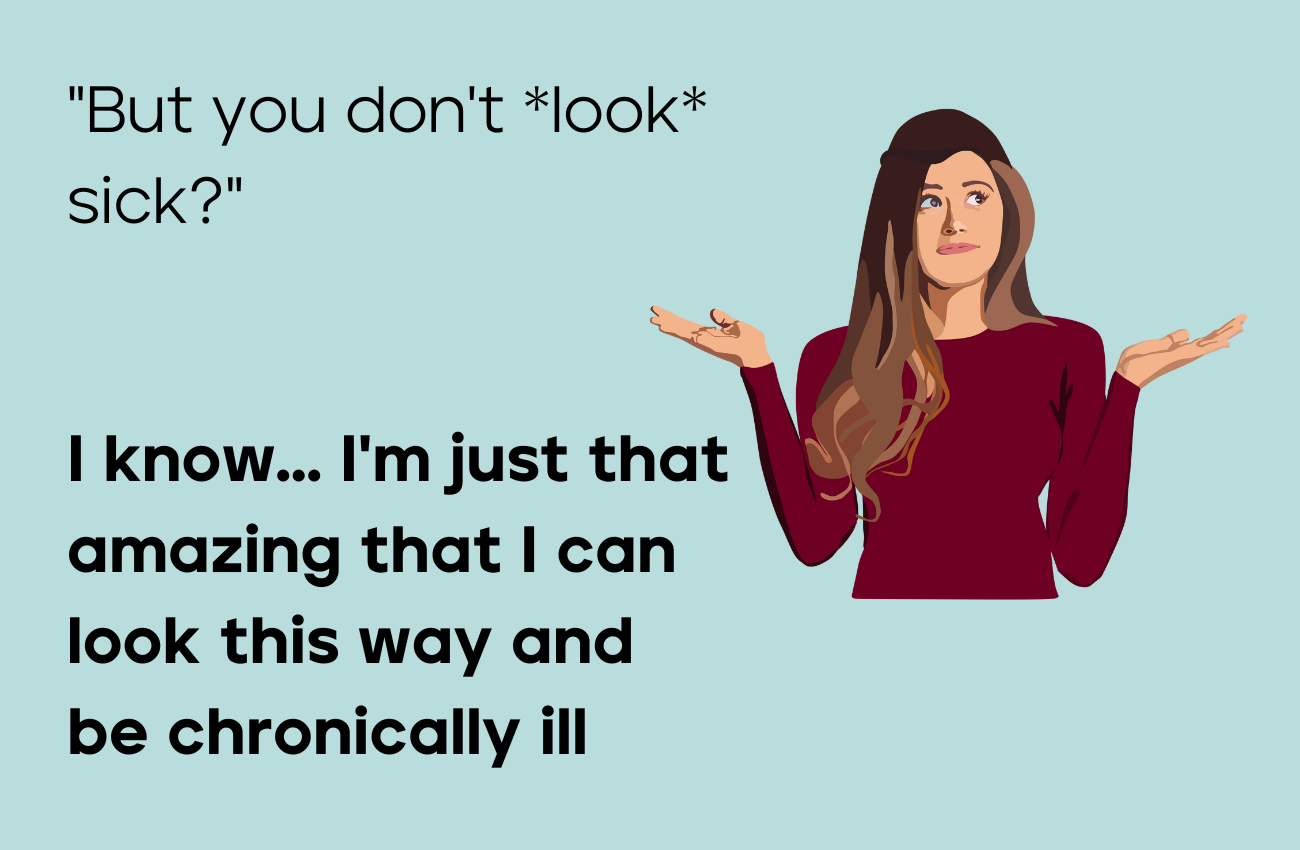
In addition to the obvious difficulties of managing the pain, fatigue, and other symptoms associated with their condition, patients with an invisible illness must also cope with emotional and psychological difficulties resulting from the fact that other people may not easily acknowledge or understand their condition. How a person with an invisible illness looks on the outside may completely misrepresent how they feel on the inside.
List of invisible illnesses
Chronic conditions that are commonly termed invisible illnesses include:
Inflammatory Conditions like Long Covid, POTS, ME/CFS, and Fibromyalgia
Autoimmune Conditions like Sjogren's, Rheumatoid & Psoriatic Arthritis, and Lupus
Gastrointestinal Conditions like IBD, Ulcerative Colitis, Crohn's Disease, and Celiac Disease
Thyroid Conditions like Hashimoto's, Graves' Disease, and Hypo- or Hyper-thyroidism
Neurological Conditions like Migraines and Multiple Sclerosis
Women's Health Conditions like Endometriosis, PCOS, and Pelvic Inflammatory Disease
Mental Health Conditions like Depression and Anxiety
How common are invisible illnesses?
Invisible illnesses are much more common than most people think, simply because it is hard to tell who has one and it can be difficult to reach a formal diagnosis. The combined prevalence of just the inflammatory, autoimmune, gastrointestinal, thyroid, neurological, and women’s health conditions listed above is ~140m Americans. Co-morbidity (when an individual has more than one condition) rates do reduce the true total of individuals with these invisible illnesses. Even so, there are likely at least 85m Americans with an invisible illness, 75% or more of whom are women.
Here are estimates of the number of Americans with an diagnosed or undiagnosed invisible illness (this list is not comprehensive):
Inflammatory Conditions
Autoimmune Conditions
Gastrointestinal Conditions
Thyroid Conditions
Neurological Conditions
Women's Health Conditions
Challenges of living with an invisible illness
In most areas of life, seeing is believing. Invisible illnesses fly in the face of this common sense notion because they do not present many (or any) obvious visible markers of the underlying illness. Consequently, people with an invisible illness must deal with a variety of frustrations and struggles, including:
Constantly having to explain to others that we have an invisible illness and what it means to have an invisible illness
Our own friends, family, and acquaintances failing to understand that just because we don’t look sick on the outside, does not mean we are not in fact sick on the inside
Our doctors trivializing their concerns because their symptoms aren’t visible, or being made to feel that our symptoms are “all in our head” (aka “medical gaslighting”)
Long and winding paths to reaching a diagnosis for our illness (for autoimmune conditions, this is ~5 years and ~5 doctors)
Dynamic symptoms, which mean some days are better or worse than others
In addition, people with an invisible illness must face the everyday difficulty of managing chronic symptoms that typically do not ever fully go away. The Spoon Theory clarifies the ongoing difficulty of living with a complex, chronic condition by using an analogy. Imagine living with a small, finite number of spoons. Every activity in a given day, no matter how small, requires a spoon, and once all of the spoons have been used up for the day, no additional activity can be done. This is what it can be like for people with a chronic condition who must carefully conserve their finite wells of energy to get them through each and every day.
In combination, all of these challenges inherent to living with an invisible illness can negatively impact the mental health of people with invisible illness, possibly increasing the likelihood or severity of depression.
How to support someone with an invisible illness
First, know that how we appear is not necessarily representative of how we feel. In other words, what is most important is that you believe someone when they say they have an invisible illness and believe their description of how it impacts them and their life.
See here for a full guide with tips on how to support someone in your life who is living with invisible illness. And here is a quick rundown from that guide of the key steps to providing support to someone with an invisible illness:
Believe them
Validate them
Offer to help them to seek care
Advocate for them and support them advocating for themselves
Educate yourself on their condition
Take care of your own mental health
How to learn more about invisible illness
Resources for gaining more knowledge about and awareness of what it means to have an invisible illness include:
Podcast: The Uninvisible Pod
Social Media: view posts with the hashtag #invisibleillness on Twitter, Instagram, and TikTok to tap into the active online patient communities
How Chronius Can Help
If living with chronic illness feels like a full time job, you aren’t alone.
That’s why at Chronius, we make it easy to navigate the healthcare system as a patient. Our online care management platform brings together all of your health records and offers a 1-click appointment prep tool that easily synthesizes your health story for your care team. You also can track all of your symptoms, identify trends, learn from vetted medical information, and follow a custom patient journey map. Plus, if you needs hands on support, our Care Advocates are available to help you with any issues you may hit up against. Personalized support as you navigate your care journey is what we are all about.
Interested in learning more and signing up for our waitlist? Claim your spot today.